BM(Hons) MD FRCS(Neurosurgery)
Consultant Neurosurgeon
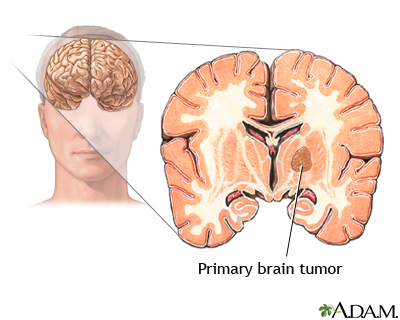
A primary brain tumour has grown within the brain from cells present in the normal brain. They can arise from any cell type but most commonly arise from supporting cells (glial cells) rather than the neurones themselves. These tumours are called gliomas. There are a number of different glial cells in a normal brain, therefore, there are different types of glioma, as indicated below. Some tumours contain more than one cell type (e.g. oligo-astrocytoma).
| Cell of origin | Tumour |
| Glial cells Astrocyte Oligodendrocyte Ependymal cell |
Gliomas Astrocytoma Oligodendroglioma Ependymoma |
| Neurones | Ganglioglioma Ganglioneuroma |
| Pineal cells | Pineocytoma Pineoblastoma |
| Reticuloendothelial cells | Primary cerebral lymphoma |
| Vascular cells | Haemangioblastoma |
Tumours are also graded from 1-4 on their rate of growth (and other features) using a system called W.H.O. (World Health Organisation). Grade 1 tumours are the most slow growing (benign) and grade 4 are the most fast growing (malignant). Some tumours have specific names:
View PDF of WHO classification of brain tumours 2021.
Unlike cancers elsewhere in the body, even the most rapidly growing malignant primary brain tumours do not tend to spread to other distant sites (metastasise). However, all primary brain tumours grow by infiltrating and invading the surrounding normal brain. Therefore, even if the surgeon removes what appears to be the whole tumour there will usually be small nests of tumour cells left behind amidst normal (functioning) brain tissue. This is why it is impossible to completely cure most gliomas (grade 2-4) and patients may need other treatments, such as radiotherapy.
It is possible to cure many grade I tumours if the surgeon is able to resect the entire lesion.
The best treatment for brain tumours depends on many factors.
The best treatment, therefore, varies from one patient to another. For some patients there may be no need for any treatment at all; in others it may be advisable to have a combination of treatments e.g. surgery, radiotherapy and chemotherapy.
The optimal treatment for each patient is now determined by a panel of specialists in most neurosurgical units in the UK. This panel (multi-disciplinary team - MDT) will consist of neurosurgeons (with specific expertise in brain tumours), neuro-oncologists (specialists in radiotherapy and chemotherapy for brain tumours), neuroradiologists (specialist in interpreting brain scans) and neuropathologists (make the diagnosis by examining the biopsies under the microscope). This opinion will be discussed with the patient by his treating doctors (often a neurosurgeon initially) but ultimately, only the patient can decide which treatments he wishes to undergo.
If your scan is suspicious for a primary brain tumour, your doctors will usually refer you to a neurosurgeon who will discuss your case with the MDT. You will then have a consultation with a neurosurgeon who will advise you of the treatment options. He will normally inform you of the importance of determining the precise diagnosis, which will involve an operation to take samples of the tumour and send them for analysis by a neuropathologist. This may take the form of a biopsy alone, or an operation to remove most/all of the tumour (see operations). The type and grade of the tumour will then determine your further treatment.
The prognosis depends primarily on the type and grade of the tumour. It is also influenced by age, general health, symptoms, the size and location of the tumour, and the extent of the tumour removal. Your neurosurgeon will be able to give you a more clear idea of prognosis when the final diagnosis has been made.